This story focusses on two tests performed at the “Clinical Laboratory Medicine” lab of Royal Liverpool and Broadgreen University Hospitals NHS Trust, http://pathlabs.rlbuht.nhs.uk/, see their “instruction sheet” http://pathlabs.rlbuht.nhs.uk/insulin.pdf (reproduced as jpeg image above).
Two babies are supposed by the prosecution to have received a huge unauthorised amount of insulin. Moreover, it was alleged that Lucy was the perpetrator of this, though how she had done it is totally unclear. For reasons which are still unclear, Lucy’s defence did not contest the first claim, obliging Lucy herself to agree with the prosecution that there must have been a murderer on the ward.
These two cases are the only cases where the jury (though reduced in size to only 11 persons) was unanimous in accepting the charges made by the prosecution. Together with the infamous post-it note confession and the infamous spreadsheet showing that Lucy was always there whenever the prosecution alleged that she had murdered or attacked babies (it would have been very surprising if that had not been the case!) these three pieces of evidence seem to be the ones which sway most people’s minds.
I recently came across a long analysis of the two insulin cases on one of the FaceBook pages devoted to the Lucy Letby trial. I believe it has been written by someone in the nursing profession. They appear to me to be extremely knowledgeable. I will reproduce the text verbatim, in a moment.
Notice that the insulin attacks are supposedly proved by the results of blood test which were requested by a doctor who apparently never looked at the result. These results were discovered either by Dr Breary or by Dr Dewi Evans (they both claim to have been the one who did this) in 2018, after the police investigation had been ongoing for a year. Note that that investigation had started almost immediately with Dewi Evans’ analysis of the medical notes on 32 incidents (deaths and resuscitations) in 2017.
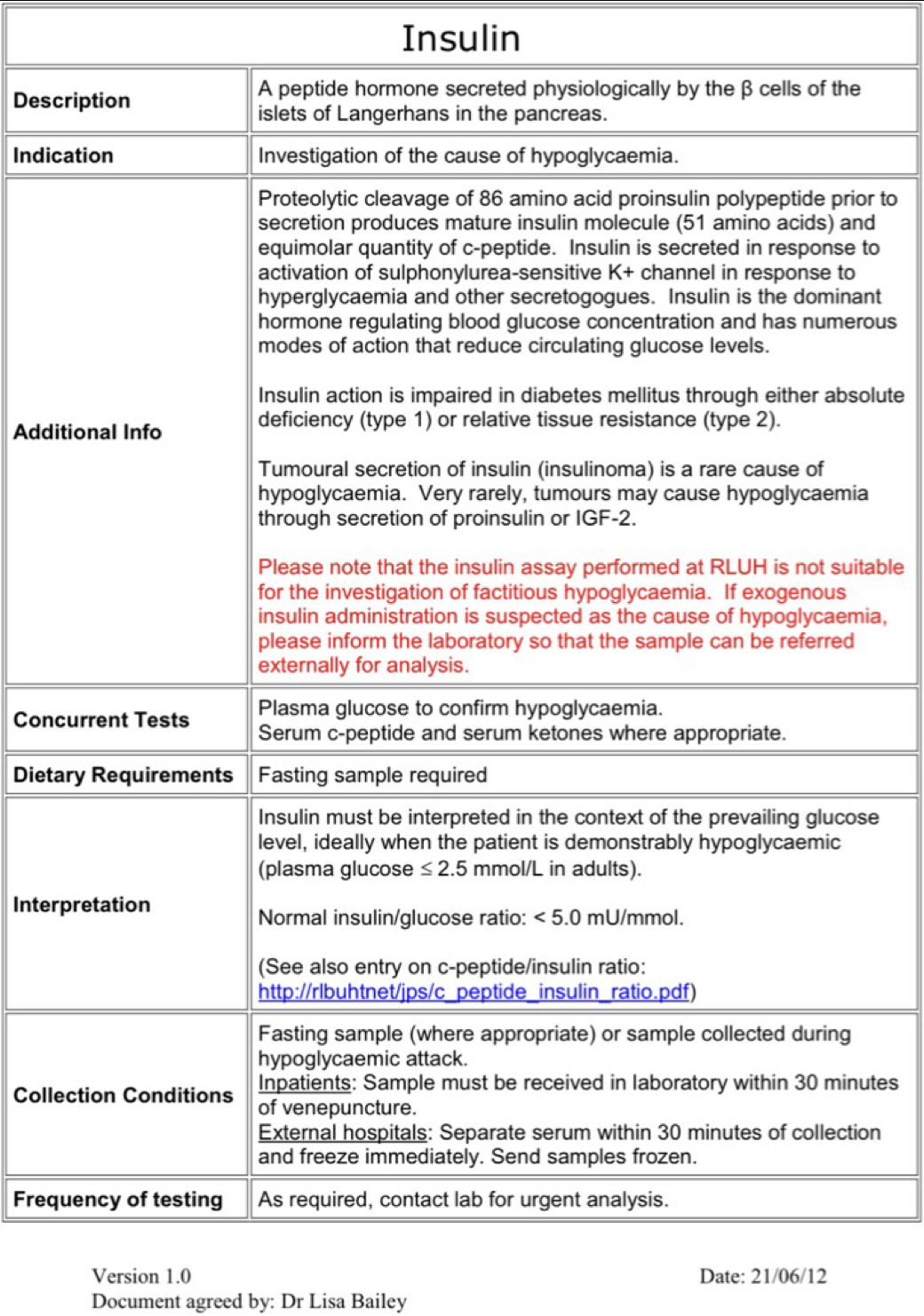
The blood test was performed by laboratory of the Royal Liverpool Hospital. The image featured at the top of this post is the information officially provided by the hospital about this particular assay. Note that it explicitly says that the test is not appropriate for the purpose it is now being used for, namely to use a high ratio of insulin to C-peptide in the blood (relatively too much insulin) as an indicator that excess insulin has been administered.
Part 2, September 21
Part 1, September 1
============================
PART 1
The now infamous INSULIN CASES.
Novel alert!
Sorry, it can’t be helped as there’s so many places to go with this. Promise I’ll try and keep some structure and attempt not to miss anything.
But you may need a drink and a comfortable seat. Let’s go.
I’ll start with some scene setting:
In August 2015 and April 2016, two separate blood test results revealed instances of two neonates who had high levels of insulin and low levels of C-peptide, in blood samples taken at the Neonatal Unit at the Countess of Chester Hospital.
The children concerned were referred to as Child F and Child L as part of the trial of Lucy Letby, due to the court-imposed reporting restrictions, protecting the identity of the babies and their families.
They are now 8 and 7 years old respectively.
The ‘insulin’ charges are considered the ‘smoking gun’ evidence against Lucy.
This is because in the majority of cases where high insulin levels are secreted naturally by the body, there will be an accompanying level of C-Peptide.
However, C-Peptide levels are not influenced by exogenous insulin levels or ‘injected’ insulin.
Hence the conclusion drawn by the prosecution.
But NOTE:
1. Where insulin antibodies are present, transiently (from for example a diabetic mother in utero) or chronically the test used will also report in the same way.
2. There are other conditions that can also generate a misleading conclusion of ‘facticious hyperinsulinism’ from this testing.
3. They include infection, primary or secondary adrenal suppression (Addison’s), genetic variants and liver issues. We do not know how much or how often.
5. The test is also unreliable in some other circumstances, including chronic kidney disease, consumption of certain drugs and alcohol as well improper sample storage/processing.
We are told that the blood results were not noted until the police investigation – with the discovery taking place at some point in 2018, a year into the enquiries by Cheshire Police.
This is important because it makes no sense and is contradicted in testimony. But let’s pretend we believe it.
How this came to pass is in itself a changing story, with both Dr Brearey and Dr Evans claiming they spotted it in 2018.
I’ve asked before what a party in the investigation, if it was conducted as robustly as the police claim in the ‘Operation Hummingbird’ documentary, who therefore should have been a suspect at this point, was doing reviewing and preparing files for the police and supposedly impartial expert witness, but this is one of many extraordinary aspects to this case.
But let’s get back into the testing.
A key point to note first is that we have no idea of how many other babies could have had the same results, as that information is not shared as part of the case put before the court.
These are not standard tests done from the off and were an external test conducted by the lab at the Royal Liverpool.
They are only ordered with persistently low blood glucose values and have to be requested by a consultant.
In neonates, hyperinsulinism as it’s known, when there is a high insulin reading, NOT related to administration of synthetic insulin, is considered rare, accounting for 1:25k births according to official data.
Although blood glucose issues more broadly are extremely common in premature babies (as confirmed by the prosecution’s chief witness himself, Dr Dewi Evans, in his post-trial interview – nice when we agree on something 😂).
Causes vary and we do not know how many others would present like this, given as per the note above, insulin and C-peptide levels are not recorded in every instance, as the resulting hypoglycaemia can resolve before it gets to that stage.
Where they are, it may not result in a diagnosis of anything – as we see in these cases, if it has corrected.
That said, it is also more common in multiples or in a sibling of a child who has also had the condition; and both of these cases relate to twins.
In both cases their sibling also had issues with maintaining stable blood glucose values.
NOTE, As a result of this, both Child F and his twin brother E were also previously prescribed insulin as part of their care.
We know from research that Transient Hyperinsulinism is often diagnosed in infants of diabetic mothers or mothers with gestational diabetes.
We know this is the case for Child L (& M), whose mother was T1, but do not know if relevant for the other set of twins.
We do not know if she is a carrier of insulin auto antibodies, or another cause for her Diabetes, such as GAD – but if this is the case, the antibodies would have been present in the twins for up to several weeks post-delivery. And alone fully explain L’s Insulin and C-Peptide ratio.
Re F, the risk of developing gestational diabetes is generally higher in people carrying twins or multiples than those carrying a single fetus, so could well be a factor for his mother.
This is because carrying multiple babies places additional stress on the body and increases the demand for insulin. The risk may also be higher due to increased placental hormones. So, it could be a factor there too.
Transient Hyperinsulinism can also occur in association with perinatal stress, which leads to Hyperinsulinism by uncertain mechanism(s).
Factors associated with perinatal stress Hyperinsulinism may include; Intrauterine growth restriction, cesarean section delivery, infection and birth asphyxia.
They also have less well-defined co-morbid test values, because there is not a singular aetiology.
We don’t know how many cases have been noted with corresponding low C-Peptide. And repeat tests can look very different given said transient nature.
Despite this – the ratio of high insulin and low C-peptide has been used to implicate many a healthcare ‘killer’, given exogenous insulin is a more common, researched explanation.
But because of these and other factors, several convictions have also been overturned on appeal. The case of Colin Norris might well become yet another example.
Both the cases for F&L would be classed as ‘transient’ as they self-corrected over time.
(Which enables us to rule out genetic causes.
So, I won’t discuss that here. Even though such tests were not completed either, but it’s more likely it would have been lasting, in all but a couple of known variants – even with treatment).
We were not given much of any comment on the risk factors in the babies involved in court, as the witnesses suggested the C-Peptide made other causes near impossible, but there are known / confirmed relevant factors, in both cases summarised:
*CHILD F* was an identical twin (to Child E) born by caesarean section (✔️) on July 29th, 2015, 10 weeks early.
Child F was just 1.434kg on delivery and had blood sugar issues from the off, before Lucy Letby was anywhere near him. He also needed resuscitation at birth and significant support with breathing thereafter (✔️).
He was being treated for an infection and ‘suspected sepsis’ (✔️). He also had ‘some jaundice’.
*CHILD L* (Twin brother of Child M) was also born by c-section on April 8 2016, seven weeks premature (✔️).
Type 1 diabetic mother (✔️).
Although closer to term that E&F, he only weighed 1.465kg, and was delivered early because the twins had stopped growing properly (✔️). Mum had been admitted two weeks prior to monitor this complication.
They had more mild breathing issues, but issues all the same (✔️).
Note Child E and F were also a set of twins for which twin-twin transfusion syndrome (TTTS) was identified.
TTTS is a rare, serious condition that happens when identical twins share a placenta (monochorionic).
Abnormal blood vessel connections form in the placenta. They allow blood to flow unevenly between the fetuses. the recipient twin receives too much blood, it can thicken.
Thicker blood is harder to pump, so the baby is at risk for developing soft tissue swelling and heart failure, and may even die in utero.
Meanwhile, the donor twin is at risk for organ failure, including the kidneys, because of inadequate blood flow.
This could be a factor in the accuracy of any blood tests taken from Child F and also a huge additional factor of perinatal stress and complications.
It’s fair to say in most reported / research cases, hyperinsulinemia is congenital (present at
birth) and is genetic.
However, children do develop the condition later and it can be transient or more lasting depending on an array of differential factors and cause.
In any case, Child F had needed insulin almost immediately after birth.
We have less accurate data regarding these cases, as they mostly self-correct. So, the numbers could also be higher than anyone actually realises.
And in fact in the neonatal period, acquired forms are usually associated with conditions like perinatal stress as noted in both babies or maternal gestational diabetes and are often transient see [6, 7] in the attached article.
Also note from the research paper linked to below:
The defining laboratory value of hyperinsulinism is not always a measurable elevation of insulin.
« Insulin levels fluctuate greatly because of the short half-life of 4 to 5 minutes and because it is rapidly cleared by the liver before it reaches the peripheral circulation »
As also seen in these babies. But put down to very different circumstances by the Expert Witnesses, with very little to back this up, years after the event.
Two important studies also ref in this paper discuss the level of plasma insulin during hypoglycemic states in large groups of patients with transient HI.
The first study noted that 22 of 27 (81%) of infants diagnosed with transient HI had elevated plasma insulin levels.
In the second study, plasma insulin levels were elevated in only 11 of 24 (46%) of neonates with transient HI.
These cases were diagnosed with hyperinsulinism on the basis of other evidence, including lack of ketosis in the setting of hypoglycemia, elevated glucose requirements, and glycemic response to glucagon.
Meaning others could fly under the radar and tests taken very close together can vary greatly.
But also is very important because of the prosecution’s allegations about why the insulin levels were high and the method they theorise exogenous insulin was administered.
So what was the cause in these babies, how was it determined, confirmed and is it as clear cut as the prosecution make out, for their lynchpin cases or ‘ah ha moment’ as they’ve put it prior.
The fact is – we don’t know. And I’ll tell you why.
The clinical pathology is not there conclusively with the testing they did and then onwardly didn’t do (esp. with the compounding factors I’ve outlined above) and well their version of events from a bigger picture perspective makes even less sense.
We have discussed this a lot from different perspectives, but I wanted to share my own personal observations – along with a video, showing that after the trial, the key parties don’t seem to be able to make their minds up how they even came across this information and who interpreted it.
Firstly – We are supposed to believe that even by the first incident, but certainly by the second, ‘the doctors’ were highly suspicious of either grave incompetence (in addition to their own – well documented in a series of reports and in court testimony) or nefarious activity by LL.
Yet astonishingly they want us to believe in the next breath, that on neither occasion the test results highlighting raised insulin levels were escalated to senior consultants.
So let’s get this straight:
They have ordered the tests for both children. They were supposedly concerned they had mistakenly or purposefully been given insulin or had some apparent disorder / wider issue with their blood glucose, endocrine system or genetics even, to have done so, over and above the standard testing at the hospital … but they didn’t think it in any way important to review the results properly at the time. 🤯
“None of us regrettably realised two babies had been poisoned by insulin, so we didn’t have the full picture”
A statement made Dr John Gibbs in court and widely shared in the media.
I’m sorry … that does not wash with me.
Nor is this what happens in clinical practice. Or rather, in any case should happen.
Talking about the first incident relating to Child F, we were told that the long and short of it is:
A blood sample was sent to the Royal Liverpool Hospital for analysis which confirmed the insulin detected was not naturally produced.
Dr Gibbs said in court on the 24NOV22 the insulin c-peptide reading should be at 20,000-40,000 to correlate with the insulin reading in his test (4657).
And so Child F had been given a pharmaceutical form of insulin administered, and he “should have never received it”.
A bold statement.
Yet Gibbs or any other prosecution witness has provided absolutely no conclusive evidence that this was the case as I’ve said.
Other than a test that does not record the type of insulin or differentiate from the insulin produced naturally by the body. Just an indicator in C-Peptide to insulin ratio, that further testing is required to investigate the cause.
Exogenous insulin one cause. Yes, the most common cause. But not the ONLY cause.
And both babies had significant risk factors for other causes as I have outlined.
So, no. That is absolutely not what the test said. Or measured. It’s a total misrepresentation.
In fact, the lab themselves suggested further testing to conclusively determine this in the results provided.
More so, (see video, link to be added later), even test interpretation notes suggest insulin autoantibodies as a potential cause.
It’s important we deal in facts, not opinions here. Especially in matters of such importance.
And we actually heard days and days of testimony re these two babies. But also, insulin and TPN, from various witnesses.
Whilst I’ll go as far as to say some of them over played their hand and made it sound like it was the only explanation, some of the experts did give a more rounded representation when pushed, a ‘most experts agree’ type statement – insinuating that there are other causes and possibilities. Even if they were presenting what they believed to be the most likely explanation (according to the prosecution case).
It’s fair to say though, no real detail was covered re other causes of Transient Hyperinsulinism in neonates, with low accompanying C-peptide, nor medical history of the mother to confirm or discount transient insulin auto immunity or great detail about the reliability of the testing when used alone to be diagnostic.
But I’ll be clear here. That is not what they were there to do.
They were hired to theorise and explain the how. The why had already been decided.
More so they brought in other experts to expand on their theory – with scientific calculations, pertaining to half-life & most likely method of administration as a result (TPN bags they claimed), but again with no real evidence that seems to stand up when you take a step back.
1. There were no TPN bags tested or retained.
2. There are many practical flaws to this. Including TPN being changed when LL was not even working a shift – with the clinical state continuing. This had them theorising that she must have ‘spiked’ stock in the ward fridge, using the bag ports.
Professor Hindmarsh for the prosecution said that insulin could be added “fairly easily” through a portal that’s located at the bottom of the feed bags.
He also told the court that in his opinion, to produce the blood glucose levels detected, around at least three or potentially four bags could have been contaminated.
Forgetting to mention that the same stock bags were being used for other babies on the ward.
It would be a starting coincidence that only one baby would have received all of the contaminated bags, eh?
Crucially though, remember they have not and couldn’t discount other causes with actual testing, or confirm if it was indeed exogenous, incl. the brand/type/chain to confirm it was the same that was held in the ward fridge, as they didn’t bother to do it, and so have no actual conclusive proof of their theorised accounts.
However much they double down.
This is the test they would require to confirm the aspect of their theory that it was exogenous or manufactured insulin and which type:
LC-MS/MS testing.
This would have not only identified if the beta chain was synthetic, but also the manufacturer of that synthetic insulin.
If negative; other avenues should have been explored, including genetic, auto immunity of various types. Transient or chronic.
But they didn’t even repeat the first test. Let alone do more.
Let summarise so far:
CHILD F had significant risk factors for congenital hyperinsulinism.
As did CHILD L, which I’ll get to shortly in a little more detail.
These risks were actually increased by over 300% due to their size and weight according to various studies.
But the prosecution claims a murderous serial killer nurse was far more plausible, despite being many times rarer on a population level than congenital hyperinsulinism. Even without the elevated risk factors.
Not even 1:300k in the U.K.
And other staff had to select the supposedly spiked TPN, for the same babies, in each case, consistently around 3 times, when LL was not on shift.
Ok.
But that’s not even it.
This is where it gets very interesting re F.
Child F collapsed on the 5th August.
Dr Gibbs, now famous here for his ‘memory’ lapses, (that only he’s allowed), conceded in his testimony to the court that insulin was given far later than originally represented in his statements (the night of the 4th August – a bolus he says) to said baby.
He had originally stated that Child F had last been prescribed insulin on the 29th July.
This was repeated by multiple professionals, each stating that none was administered since the 29th July.
Which for me makes all of this completely nul and void. Their records were a mess. How do we know that any of it was reliable.
The child had insulin.
More so, F’s brother, Child E WAS prescribed insulin too.
Child E had sadly passed the prior day, but obviously has the same surname.
Was this a matter of incompetence?
Is it not more plausible that IF the result was indeed due to synthetic insulin, that Gibbs did only give a bolus overnight if we can believe his latest conclusion.. that further doses could have been given in error, to a child with the same surname, right next to F?
Especially on a chaotic ward making an exceptional number of mistakes, that have been well documented.
To make this seem unlikely … it was represented to the court that there were no other children on the ward, in receipt of insulin at the time. Technically correct, but also misleading on account of this information.
So, what about the sequence of events relating to the results?
Evidence was also given to the court that the results for Child F were phoned through to the Countess of Chester’s biochemistry lab on August 13. (It is a delayed result).
By that stage Child F’s blood sugar had stabilised and he had been moved to a different hospital closer to his parents’ home.
So, NOTHING was followed up.
A doctor involved in the care of Child F said she was “at a loss” to explain the blood test findings.
The medic, who could not be identified for legal reasons (convenient eh!), told Manchester Crown Court:
“This is something we found very confusing at the time because (Child F) had only been prescribed insulin five days previously (on July 31). AGAIN even though Gibbs changed his story on this date.
Contrary to the account of Dr Gibbs and Dr Brearey, the unnamed doctor said it was looked at to see if anyone else at the time was prescribed insulin in the whole neonatal unit. Investigated for a possible ‘accidental administration’, when the results came back. But there were no other babies at that time. No further action was taken.
Ummm.
Gibbs claimed that ‘I was not thinking at the time that someone might have administered insulin. The results showed that, but unfortunately the junior doctors who read them didn’t realise the significance’.
Seemingly contradicting her. She clearly DID understand the potential significance.
So what was it … Who is telling the truth?
They need to get their story straight.
But from this we can infer they did know … or why did they check the other prescriptions?
And so Gibbs and his bolus aside, if they had this information, why didn’t they follow the advice to understand WHY these tests came back as they did?
So let’s get to Child L, where denials and excuses become even more astonishing. By now we are in APRIL 2016.
The doctors were in full ‘blame Lucy’ mode and had been in conflict with management.
A blood sample taken from Child L was again sent to the Royal Liverpool for the tests.
That too showed a high level of insulin which the prosecution and the media tell us ‘had been given to the patient’ again with absolutely no evidence, other than some clever sounding, educated theory that it was the case.
For all the same reasons it’s disingenuous to claim otherwise..
Even more so with Child L’s mothers T1 diabetes. There was even more likelihood of a biological rationale for the events.
YET AGAIN – The result was phoned through to the Countess of Chester on April 14 and entered on the computer system – with no further action taken that was tangible or followed the next steps suggested by the lab.
Crucially again … it’s Doctors ordering these tests. They don’t order themselves and procedure states that they have to be both requested and interpreted by a consultant.
Why were we not given more specifics here?
Who did this.
Why were we not given the name of the doctor that both ordered and interpreted the tests?
Why was this and procedure glossed over?
Why were doctors allowed to make inaccurate statements unchallenged?
The media happily minimise phrases like “it significance did not appear to be appreciated as the child’s condition had improved”.
Ummm, not good enough. And highly misleading.
Now let’s briefly discuss the numbers for each baby. As it opens another worm hole.
For Child F the insulin level was provided to the court as 4657. I am presuming this is pmol/mL – as despite this being INSANE, any alternative unit measurement is worse.
Note, 4000 anything insulin, is enough to put grown man in a coma.
It would not be unreasonable to conclude this is likely to be inaccurate. And would call for repeat testing.
In fact, generically neonatal blood tests often read inaccurately high, on account of low blood volume and potential newborn hemolysis, so often need to be repeated.
Confirmed now by several doctors.
Where there is TTTS even more so.
For Child L, it was far lower.
1,099. With a smaller C-Peptide disparity (recorded as 264).
Remember this is the child with a type one diabetic mother.
Given the values are not just significantly lower, but in another stratosphere – would it not make more sense to conclude that they were not the result of the same set of circumstances. And that this is more likely the cause of the hyperinsulinism with low C-Peptide?
Now blood sugars.
In both cases some of the many values given were not even indicative of poisoning.
Levels of 0.2 or lower – would be expected.
In Child L, they never fell below 2.0. Not once.
In F, the lowest reading was 0.8. But others were much higher.
I’m not going to go too much into the chain of evidence as it’s a lesser factor. But we don’t know what happened in transit to the lab. Bloods without this clearly documented can become inadmissible evidence in any case.
That’s before we get to both the TPN and insulin. Even after its arrival on the ward from all over the contentent and via various hospital departments, the entire ward staff had access to it. Yet of course, if it went as told, it had to be LL. I won’t even give this any more time. 🥴
And let’s get back on to Dr Evans and the police now.
The police claim that Dr Evans reviewed all files relating to collapses and deaths of babies covering the period in question (June 2015-July 2016, when Lucy was removed from the ward) to determine which were ‘suspicious’.
However, Dr Evans claimed in his post-trial interview, that he only saw the files for F&L, because their siblings were “harmed in other ways”.
So … why were their collapses not included in the original bundle?
Is it because Lucy Letby was not on shift in the most part, so the files had been ‘pre sifted’, to only include babies that collapsed or died when Lucy was on shift?
Can we reasonably infer from this that they were ever only investigating incidents they could associate with Letby being on shift, despite their claims to the contrary?
Which also makes their so called ‘strongest evidence’ their potential undoing. Well, the undoing of their narrative in any case.
Especially since as no information was provided in discovery as to the other up to 10 deaths (numbers vary from different sources as we have previously discussed, which in itself is a 🚩) and unknown number of other collapses in the same 12-month period.
Or indeed what really differentiated these from the others – with the very vague and unshared methodology of ‘unexpected and unexplained’.
Despite all the cases linked to the charges, having many, many factors that regularly cause death and collapse in premature infants.
The police want us to believe that deaths and collapses in neonates is exceptionally rare.
10 others on the same ward and statistics re mortality by gestational age (see my prior posts), also prove this a fallacy. Even if these comorbidities did not exist.
In what sort of alternate reality is this acceptable?
#Mils
=================================—
PART 2
The insulin debate.
First, let’s repeat the beginning of the Part 1.
Discordant Insulin to C-peptide results being an absolute indication of factitious insulin administration is an entirely false assumption.
Not only that, the results proposed are beyond insane.
There are several reasons for that, it’s complex and multifactorial.
Let’s try and break it down somewhat.
• The test showed that the insulin concentration was 4657/pmol/L, the C-peptide was 169 pmol/L and the glucose was 1.3 mmol/L. Within two hours of the blood test the baby’s blood sugar level was ~4 mmol/L, which is normal.
• When there’s is a concern of neonatal glucose issues, the best standard of care would be to take C peptide/Insulin levels from cord blood at birth or at first recognition of an abnormal blood sugar, or when there is known diabetic mother either – Type1/2 or gestational. It’s a right away job. Not a ‘when shit hits the fan’ job.
• Second from that, the test to prove exogenous insulin is preferably done fasting, though ovbiously impossible in neonates, it can also be done in the first instance of sudden, unexpected hypoglycaemia. This would be differentiated as a ‘fasting’ result and a ‘stimulated’ result.
• However, what you don’t do, what you absolutely avoid doing, if you want any accuracy or legitimacy in the results, you later use to infer attempted murder – You do not start treating the hypoglycaemia, then take the C peptide/ to insulin test. A test taken after treatment has commenced, is completely compromised.
• Because treatement of hypoglycaemia raises the insulin and suppresses the C peptide, therfore you get abnormal results.
• The hypoglycaemia was treated with IV dex MULTIPLE times over several hours, prior to this test being considered, returning an odd result. If it were to be considered a legitimate result. It would insinuate invalidity, due to not being taking prior to treatment. Those results could be partially explained by the repeated IV dex prior to the test, which stimulates the Insulin release and supresses the C peptide.
And now Part 2 really begins –
• DR Gibbs states the patient is peripherally shut down. And blames possible infection or stress. Yet that is also a consequence of Hypoglycaemia. Hypoglycaemia induces a reduction in peripheral circulation, which in turn affects circulating blood volume for tests. Slow difficult blood draws often read Insulin inaccurately high.
• A C Peptide of “under 169 P/Mol” being considered ‘undetectable’ is also, complete randomness. 169 is not a low C – Peptide result, under 94 is the beginning of low 94 – 300 is an ‘indeterminate’ number. 300 + is high.
• It’s widely assumed that a supressed C peptide from insulin would be very low, much lower than 94, never mind 169. p/mol/l.
Though this varies in neonates,
Recent studies show that 5 out of 9 c peptide results were low, 4 out of 9 was high, after insulin administration. (it is not an exact science in the most complex creatures in this world)
• The test itself is unfortunately difficult to trust, as the standards prior to it arriving frozen, rely on it being centrifuged and frozen within 30mins of being taken. As a nurse who has worked in 4 hospitals in various departments, The likelihood this happened at 5.30am in a busy acute hospital is almost 0. I would be flabbergasted if even a good hospital managed that.
• Even if it was handed straight to the lab, it would sit amongst the ED bloods that come every 5 to 10 mins, where 1 or 2 members of staff would slowly work through them.
• Unless it was sent on a bed of ICE, the sample would have already started to degrade, it wasn’t sent on Ice, there is no Ice in the woman and children’s building. If it was centrifuged (plasma separated) after 6 hours, it would be non-diagnostic, totally void. They only confirm it arrived frozen and was processed within 24 hours. No one has confirmed it was treated and frozen within the expected 30 mins.
• On top of that, it was sent to Liverpool, who state they cannot diagnose exogenous insulin in their 2012 protocol, but on this day, on the C peptide page, have returned to their 2010 protocol which has no mention of their inability to detect exogenous insulin. (Good PR for the trial not to fully annihilate your credibility, eh?)
• The people who should be doing this test – Guilford, who they considered forwarding the sample too, but didn’t, as they had ‘confidence’ in the tests accuracy despite working off a much older set of standards for preservation.
• Guilford had a different set of standards, for neonates especially. They request the blood test of neonates to be heparinised, as there is normally a much lower blood volume and this maximises the plasma for testing.
• Had the test went to the right lab, to verify what this test is supposed to be proof of, it wouldn’t have even been in the same vial, never mind every other error up until that point.
Summary.
1. The test wasn’t done at the time needed to diagnose exogenous insulin. First episode of hypoglycaemia, prior to treatment.
2. Multiple attempts to rectify the blood sugar, would have increased the plasma insulin and supressed the c peptide.
3. The test was taken from a peripherally shut down patient who had issues with cannulation and multiple IV infusions of dex
4. The test would have needed to come from a non-IV line infusion arm or limb. Though failed cannulas would likely have meant there was no IV free limb.
5. The test needs to be kept at 4’ min immediately, centrifuged within 30 mins and frozen to -20, to stop degradation as the hospital and Liverpool lab were still using the less stable testing protocol of gel tubes. Despite there being a testing protocol that allows 24*s stability at ambient temperature.
6. If it was delayed 6 hours + prior to the centrifuge, the results were degraded and absolutely unable to be used in court. Even if they arrived to Liverpool ‘frozen’
7. They were sent to a lab unable to conduct the proper testing that would have actually evidenced exogenous insulin, the lab that accurately determines that was Guilford, the test didn’t go there. We are relying on Liverpool’s interpretation, despite them not having the proper assays to be used credibly, like to accuse someone of murder.
8. Had there have been some initiative in sending the test to the right lab in the first instance, the Guildford lab would have advised that neonatal bloods specifically, were taken in a ‘red top’ no preservative, heparinised, then separated, as neonatal blood tests cannot be treated the same way as adults.
9. HOWEVER despite all of that – 4657/pmol/l cannot be the result, it is not possible. Not on the proposed 0.6ml Of insulin added to a slow bag which is another fallacy entirely. That same result was found on attempted suicide patients who injected over 200 Units of insulin, and who were in a coma in the ICU for several days.
10. The insulin may have already been high from all the IV Dex infusions, likely a degraded, partially haemolysed sample from inability to follow the strict protocol, taken too late, from a peripherally shut down neonate, it wasn’t heparinised, as expected for neonates and small blood volumes, yet Liverpool ran it anyway.
A blood test with very serious consequences, requires it to be done properly and to the letter. Then be properly analysed considering the results make 0 sense even if insulin was added, the C peptide would have been less, the patient would have been very much dead or dying – Not recovering to a Blood sugar of 4 0 – 2 hours later
11. The C peptide result of 169 P/Mol/l is not low for neonates. It doesn’t come under the bracket of low, yes it’s lower than expected for an insulin level that high, maybe in adults? but once you start treating the issue, you supress the C peptide, so it may even have been normal, prior to all the increasing dex infusions.
Would this be good enough for your life?
#Weegie RN
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5862205/
Angelidi, A.M., Filippaios, A. and Mantzoros, C.S. (2021). Severe insulin resistance syndromes. Journal of Clinical Investigation, 131(4). doi:https://doi.org/10.1172/jci142245.
Cryer PE, Axelrod L, Grossmann AB et al. Evaluation and management of adult hypoglycaemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2009;94:709-728. This identifies 0.2 nmol/L (0.6 μg/L) as the critical concentration below which C-peptide should be suppressed during hypoglycaemia.
ECLI (2019). C Peptide (Plasma) / Blood Sciences Test / Exeter Clinical Laboratory International. [online] Exeterlaboratory.com. Available at: https://www.exeterlaboratory.com/test/c-peptide-plasma/.
McDonald, T.J., Perry, M.H., Peake, R.W.A., Pullan, N.J., O’Connor, J., Shields, B.M., Knight, B.A. and Hattersley, A.T. (2012). EDTA Improves Stability of Whole Blood C-Peptide and Insulin to Over 24 Hours at Room Temperature. PLoS ONE, [online] 7(7), p.e42084. doi:https://doi.org/10.1371/journal.pone.0042084.
Sacks DB, Arnold M, Bakris GL et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care 2011;34:e61-e99.https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Neonatal_hypoglycaemia/
Venugopal, S.K., Mowery, M.L. and Jialal, I. (2020). C Peptide. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK526026/.
www.clinlabnavigator.com. (n.d.). C peptide measurement helps to determine the cause of hypoglycemia. [online] Available at: https://www.clinlabnavigator.com/c-peptide.html [Accessed 21 Sep. 2023].
www.ouh.nhs.uk. (n.d.). Causes of spurious results – Biochemistry. [online] Available at: https://www.ouh.nhs.uk/biochemistry/tests/spurious-results.aspx.
Yamamoto, J.M., Corcoy, R., Donovan, L.E., Stewart, Z.A., Tomlinson, G., Beardsall, K., Feig, D.S. and Murphy, H.R. (2019). Maternal glycaemic control and risk of neonatal hypoglycaemia in Type 1 diabetes pregnancy: a secondary analysis of the CONCEPTT trial. Diabetic Medicine, 36(8), pp.1046–1053. doi:https://doi.org/10.1111/dme.13988.
MedicineNet. (n.d.). What Is a High Insulin Level? [online] Available at: https://www.medicinenet.com/what_is_a_high_insulin_level/article.htm

Excellent summary
Thank you